Among the Highest Heart Attack Survival in the Nation
The heart receives blood from the coronary arteries. Plaque buildup (slow progression of fat, cholesterol and calcium deposits) in these arteries is called coronary artery disease, which can lead to heart attack, stroke and death.
At Bluhm Cardiovascular Institute, experts use an integrated and collaborative approach to diagnose, stage and treat coronary artery disease. Our comprehensive therapies, offered at multiple inpatient and outpatient locations, include carefully chosen medications and advanced procedures and surgeries. "Having among the highest heart attack survival in the nation is a reflection of the high-quality and safe care we provide to our patients. Our excellent survival rate, in part, is achieved with timely percutaneous coronary intervention (PCI) when necessary, which preserves heart muscle and function,” says Ian D. Cohen, MD. |
Minimally Invasive Technology for Chronic Total Occlusion
Bluhm Cardiovascular Institute offers advanced, minimally invasive technologies for treating chronic total occlusion (CTO)—complete blockage of a coronary artery with thoroughly solid plaque (its density is often compared to concrete). Some patients with CTO don’t know they have this type of coronary artery disease or have been told their only option is to live with their symptoms or undergo major open heart surgery. Catheter-based CTO techniques now offered at Bluhm Cardiovascular Institute provide an attractive, alternative treatment option.
“Instead of suffering with their symptoms, patients who undergo this treatment frequently enjoy dramatic improvements in their quality of life,” says Mark J. Ricciardi, MD, one of only a few interventional cardiologists around the world specially trained in advanced CTO treatment. |
New Stent Technology to Treat Coronary Artery Disease
Having participated in the initial clinical trial studying the safety and efficacy of bioabsorbable stents in select patient populations, Bluhm Cardiovascular Institute now offers the latest generation of bioabsorbable coronary stents for general use by the population. A bioabsorbable stent is a temporary device which functions like a drug-eluting stent, but is not made out of metal.
“While we have had great success with drug-eluting stents, once placed in the body they remain forever. With this new technology the device is absorbed into the body after it has delivered the appropriate therapy,” says Mark J. Ricciardi, MD. |
Patient Outcomes: Coronary Artery Disease
At Bluhm Cardiovascular Institute, we evaluate our clinical outcomes so that we can fully understand how our treatments and procedures benefit our patients. We regularly review and evaluate our clinical outcomes and based on the results, develop methods to monitor and improve the health care we offer to our heart and vascular patients.
Please see below for our four coronary disease measures. |
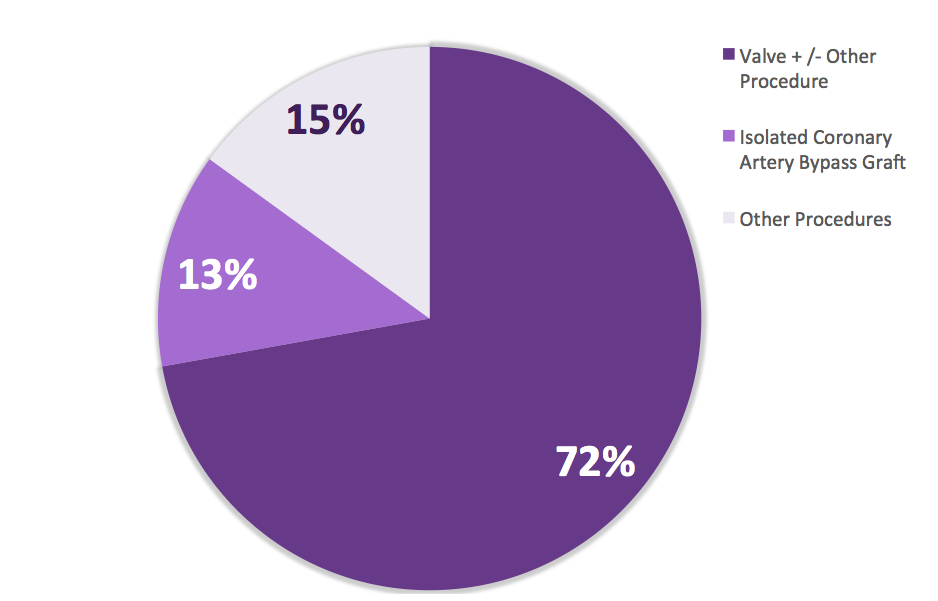
Distribution of Cardiac Surgery Procedures Highlights the Complexity of Procedures PerformedCalendar Year 2016
|
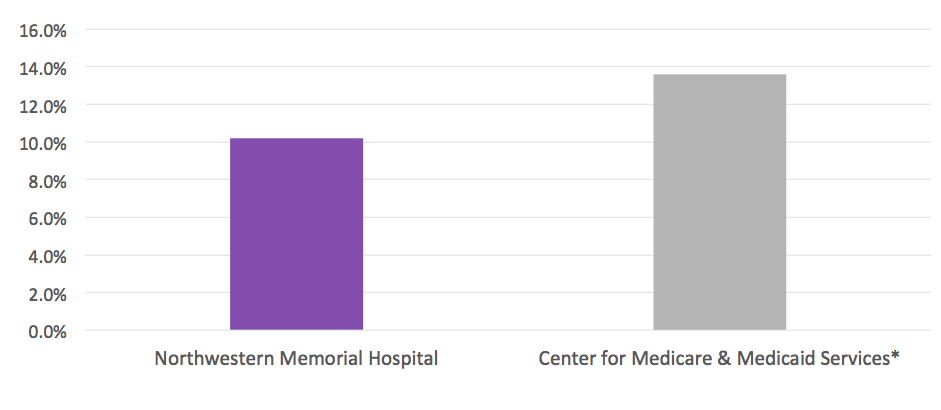
Among the Top 10 Hospitals in the Nation* for Risk-Adjusted** 30-Day Heart Attack Mortality RateJuly 2013 - June 2016
Source: Hospital Compare *Includes all hospitals that report data to the Center for Medicare and Medicaid Services. In this case lower is better. **Risk adjustment allows for a more accurate comparison by accounting for individual patient factors present prior to hospitalization such as age, severity of illness and other medical problems that can put certain patients at greater risk of complications or death than others. |
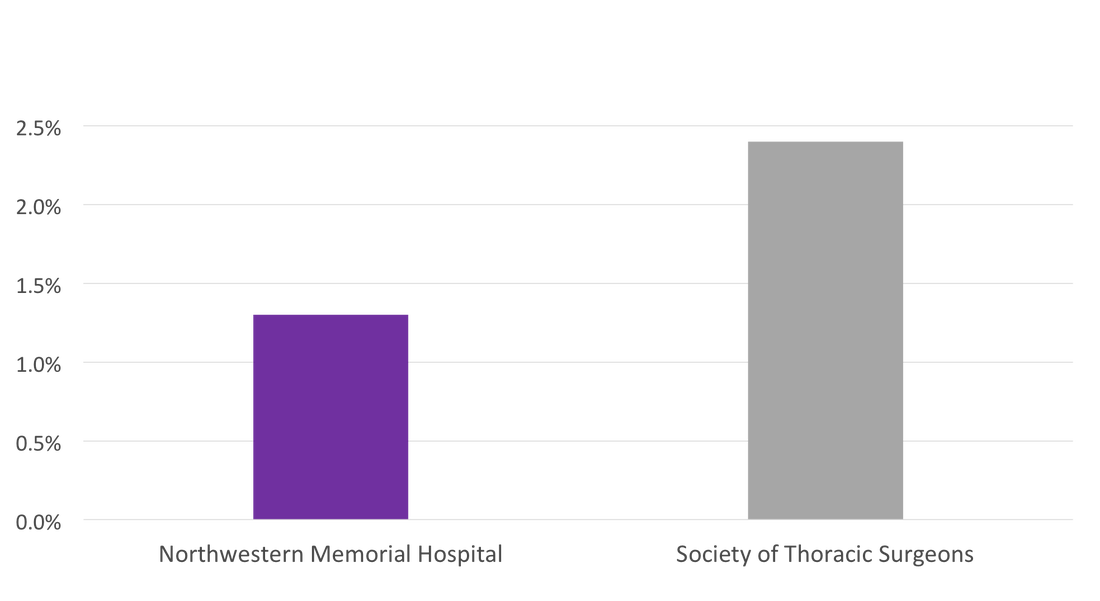
Lower Risk-Adjusted* 30-Day Mortality Rate Following Major Cardiac Surgery** as Compared to National Average Calendar Year 2016Source: Society of Thoracic Surgeons Registry
*Risk adjustment allows for a more accurate comparison by accounting for individual patient factors present prior to hospitalization such as age, severity of illness and other medical problems that can put certain patients at greater risk of complications or death than others. **Includes CABG, Aortic Valve Replacement, Aortic Valve Replacement + CABG, Mitral Valve Replacement, Mitral Valve Replacement + CABG, Mitral Valve Repair, & Mitral Valve Repair + CABG. In this case lower is better. |
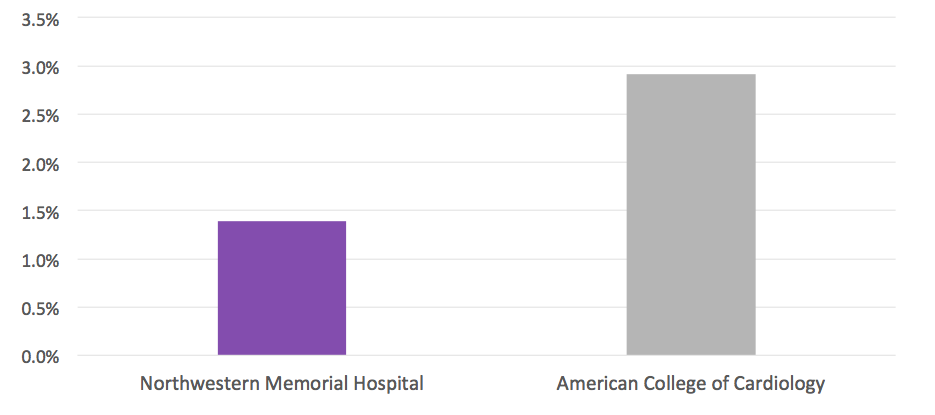
Lower Risk-Adjusted* In-Hospital Mortality Rate Following Percutaneous Coronary Interventions as Compared to National AverageApril 2016-March 2017Source: National Cardiovascular Data Registry (NCDR)
*Risk adjustment allows for a more accurate comparison by accounting for individual patient factors present prior to hospitalization such as age, severity of illness and other medical problems that can put certain patients at greater risk of complications or death than others. |
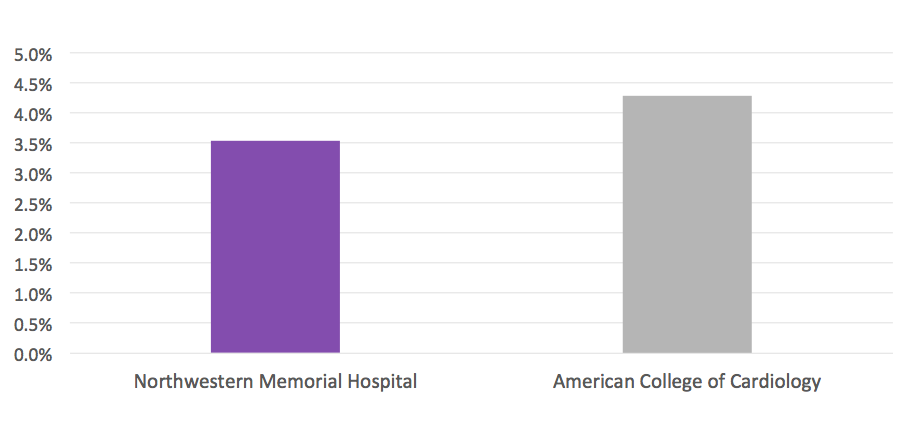
Lower Mortality and Major Complications* Rate Following Percutaneous Coronary Intervention as Compared to National Average April 2016-March 2017Source: National Cardiovascular Data Registry (NCDR)
*Complications include in-hospital mortality, stroke, emergency coronary artery bypass graft surgery and repeat target revascularization. In this case lower is better. |
Lower Risk-Adjusted* Incidence of Bleeding Following Percutaneous Coronary Interventions as Compared to National Average** April 2016-March 2017Source: National Cardiovascular Data Registry (NCDR)
*Risk adjustment allows for a more accurate comparison by accounting for individual patient factors present prior to hospitalization such as age, severity of illness and other medical problems that can put certain patients at greater risk of complications or death than others. **In this case lower is better. |
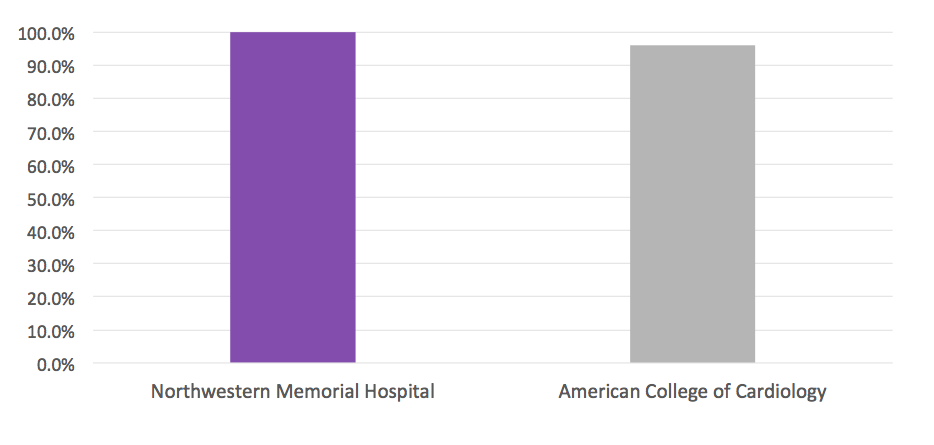
100 Percent of Heart Attack Patients* Receive Percutaneous Coronary Intervention Within 90 minutes** of Hospital ArrivalCalendar Year 2016Source: National Cardiovascular Data Registry (NCDR)
*Includes ST-elevation Myocardial Infarction (STEMI) patients; Excludes patients transferred in; patients who received fibrinolytics prior to Percutaneous Coronary Intervention (PCI); PCI indication described as Rescue PCI for STEMI, PCI for NSTEMI, PCI for STEMI (stable after successful full-dose lytic), PCI for STEMI (unstable, >12 hr from symptom onset), PCI for STEMI (stable, >12 hr from symptom onset) or Other; patients with a non-system reason for delay for PCI and a time to First Device Activation >90 minutes **To reduce mortality and complications, the American College of Cardiology (ACC) recommends that STEMI patients receive PCI within 90 minutes of hospital arrival. |
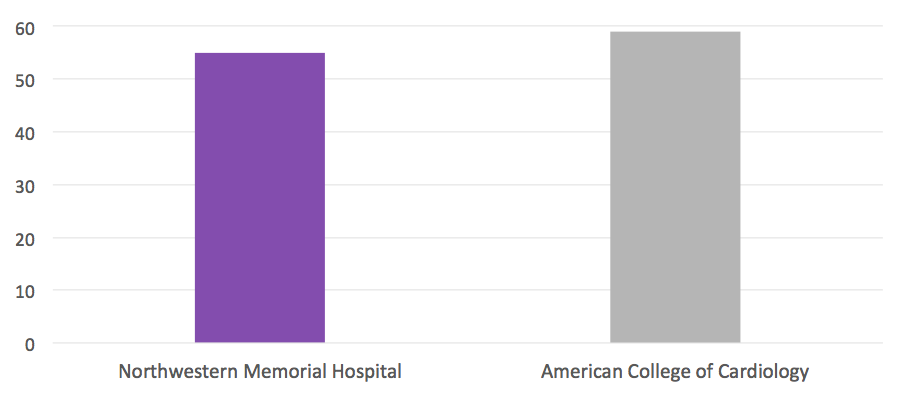
Median Time (in Minutes)* to Receive Percutaneous Coronary Intervention from Hospital Arrival Better than National Average**April 2016-March 2017Source: National Cardiovascular Data Registry (NCDR)
*In this instance, lower is better. **Excludes patients transferred in; patients who received fibrinolytics prior to Percutaneous Coronary Intervention (PCI); PCI indication described as Rescue PCI for STEMI, PCI for NSTEMI, PCI for STEMI (stable after successful full-dose lytic), PCI for STEMI (unstable, >12 hr from symptom onset), PCI for STEMI (stable, >12 hr from symptom onset) or Other; patients with a non-system reason for delay for PCI and a time to First Device Activation >90 minutes |
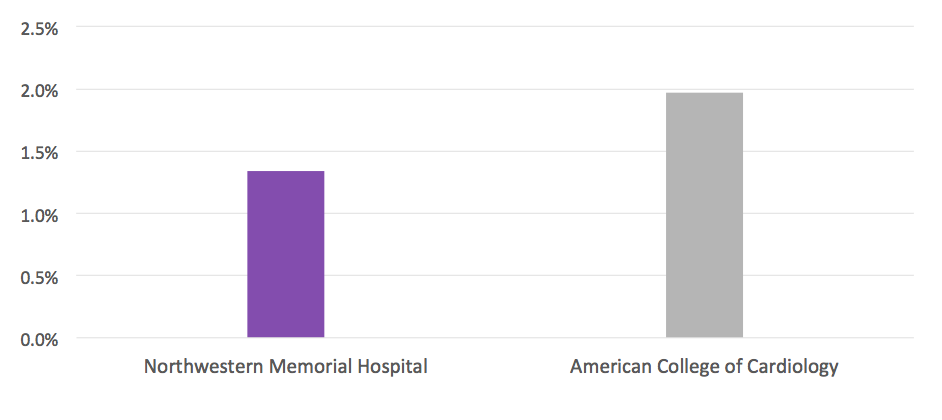
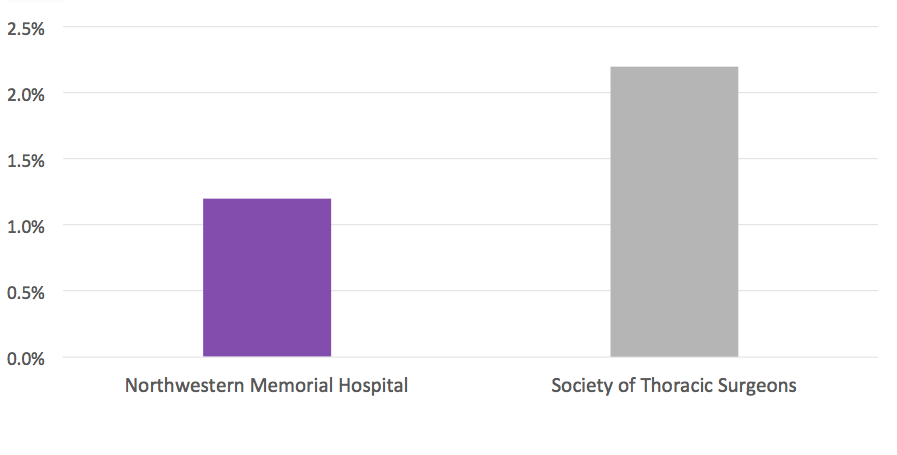
Lower Risk-Adjusted* 30-Day Mortality Rate Following Isolated Coronary Artery Bypass Graft Surgeries as Compared to National AverageCalendar Year 2016Source: Society of Thoracic Surgeons Registry
*Risk adjustment allows for a more accurate comparison by accounting for individual patient factors present prior to hospitalization such as age, severity of illness and other medical problems that can put certain patients at greater risk of complications or death than others. |
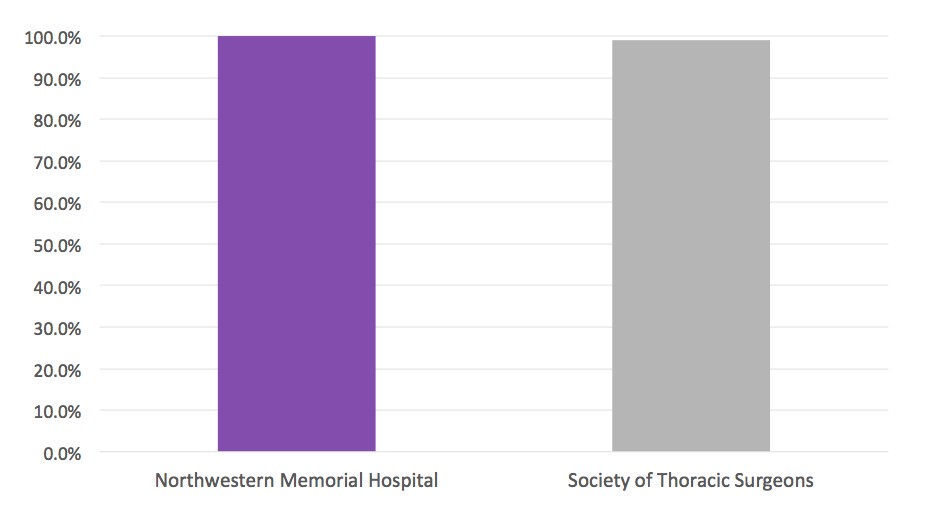
100 Percent of Patients Undergoing Coronary Artery Bypass Graft Surgery Received an Internal Mammary Artery (IMA) GraftCalendar Year 2016Source: Society of Thoracic Surgeons Registry
|
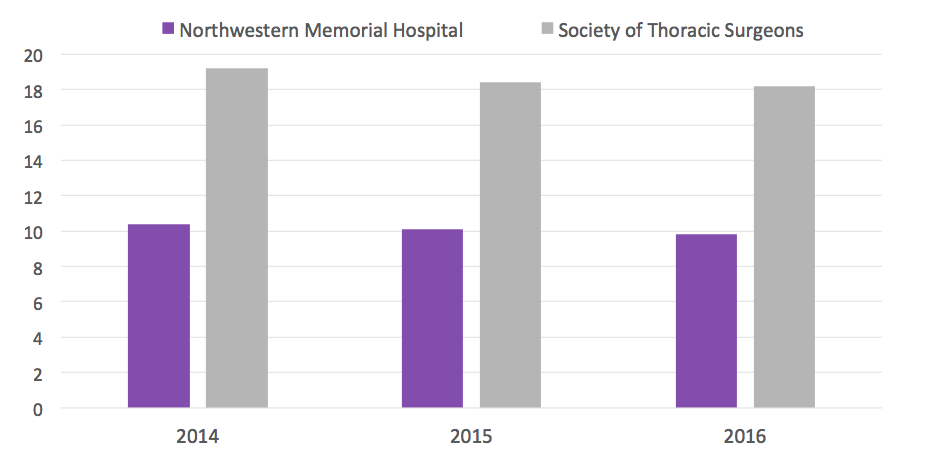
Coronary Artery Bypass Graft Surgery Patients Consistently Require Less Breathing Assistance (in Hours) from a Ventilator as Compared to National Average* |
Calendar Year 2014-2016
|
Source: Society of Thoracic Surgeons Registry
*In this case lower is better. |
|
© 2024 by Northwestern Medicine® and Northwestern Memorial HealthCare. Northwestern Medicine® is a trademark of Northwestern Memorial HealthCare, used by Northwestern University.
|